Pelvic Floor Disorders

Pelvic floor dysfunction (PFD) is a global health problem that affects millions of women and men.
The occurrence of pelvic floor disorders is proven to increase with age, but symptoms can show much earlier, and at any age. Although PFD is so common, there is still some stigma attached to seeking the right care. If left untreated, it can have a negative impact on health and quality of life.
What is pelvic floor dysfunction?
PFD is the inability to control pelvic floor muscles due to them being damaged, weakened or too tight. Pelvic floor muscles function as a hammock to support organs such as the bladder, rectum, and uterus. Its key role is to provide support and stability to these organs. The muscles are held in place by surrounding ligaments and fascia.
These muscles prevent pelvic organs from being pushed downwards when there is intra-abdominal pressure due to movements such as straining, lifting, carrying, or bending. They also help to keep the bladder and bowel openings closed.
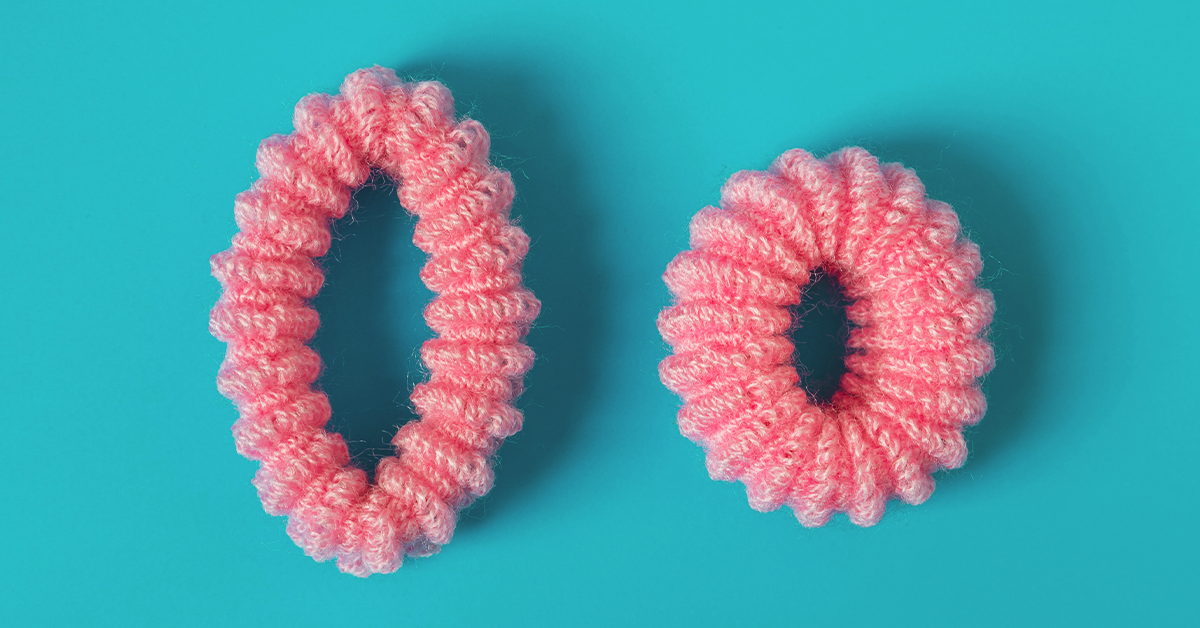
It is important to note that PFD is a broad constellation of symptoms and changes to the pelvic floor muscles, and is further classified as hypotonic (loose) or hypertonic (tight).
What is a hypotonic pelvic floor?

A hypotonic – or loose – pelvic floor happens when pelvic muscles and connective tissue weaken. There are several contributing factors:
- Advancing age
- Obesity
- Childbirth
- Injury
- Menopause or hormonal changes
- Chronic coughing or sneezing
- Surgery and treatments
The laxity of the pelvic ligaments and weakness of the pelvic muscles lead to symptoms such as:
- Urinary or bowel incontinence
- Frequent restroom visits
- Discomfort when urinating or defecating
- Accidentally passing wind when making sudden movements
- Pelvic pain
- Pain during sexual intercourse
- Reduced sensation in the vagina
- Heaviness in the vagina or rectum
Prolapse pelvic organ prolapse is experienced more by women than men. This occurs when pelvic organs start to droop and later protrude out of the vaginal opening. They can be felt, or even seen, and affect daily activities.
Physiotherapy and physical training such as ‘Kegels’ can treat hypotonic symptoms. They are beneficial to both men and women.
What is a hypertonic pelvic floor?

A hypertonic pelvic floor is when pelvic muscles are too tight and unable to relax. It can be caused by the following:
- Stress
- Certain medical conditions
- Infections
- Pelvic surgery
- Bladder or bowel dysfunction
- Gripping due to bad posture
- Certain sports and exercises
- Trauma, including sexual abuse
As relaxed pelvic floor muscles are essential to urinate or defecate, it becomes difficult to completely empty the bladder or bowels. Trips to the restroom may increase but with no relief. Due to its similarities, there is a tendency for this condition to be misdiagnosed as a urinary tract infection (UTI) or constipation.
Common symptoms that indicate a tight pelvic floor are:
- Painful periods
- Pain during sexual intercourse
- Pain inserting tampons
- Pelvic pain
- Slow urine flow and bowel action
- Erectile dysfunction
- Premature ejaculation
Ways to prevent a hypertonic pelvic floor
Many athletes suffer from a hypertonic pelvic floor because of high-impact activities that lead to overactive pelvic muscles. Individuals in sports and fitness may develop a habit of holding onto their core muscles which subsequently tightens the pelvic floor. Other factors such as trauma and stress can store tension in the pelvic region too.

The following can help to relax pelvic muscles and prevent hypertonicity:
- Manage stress and anxiety
- Practice relaxation techniques
- Breathing exercises, meditation, yoga
- Avoid holding urine or stools for prolonged periods due to a busy lifestyle or laziness
- Vibrators, vaginal dilators or pelvic wands can help to release stored tension
- Remember to “let go” when doing kegels
The idea is to acknowledge that pelvic muscles are always at play. For example, when the buttocks tighten, the pelvic muscles tighten as well. Adding pressure to the inner thighs does the same, so sitting cross-legged for hours can be equally damaging.
Men and women experience pelvic dysfunction differently

Pelvic disorders are more prevalent in women due to childbirth. Incontinence, overactive bladder, and pelvic organ prolapse are some of the more commonly experienced symptoms. Prolapse occurs due to the weakening of the pelvic floor during pregnancy as well as after birth. Every pregnancy adds stress to the pelvic floor, as it accommodates the weight of a growing baby. Both vaginal and caesarean deliveries can cause pelvic floor dysfunction, but they affect individuals in different ways. Vaginal delivery more associated with incontinence and pelvic organ prolapse, whereas a C-section has more of a link to sexual dysfunction.
Men on the other hand, may struggle with erectile dysfunction. A weak pelvic floor impairs the ability to delay ejaculation causing premature ejaculation. The prostate (which is part of the male reproductive anatomy) is located just below the bladder, and it can be inflamed causing chronic pelvic pain. Men with prostate cancer can develop PFD due to targeted radiation treatments.
Caring for your pelvic floor
Making the effort is important even when acute symptoms are not present. Forming conscious awareness can lead to small changes. Remember to,
- Pay attention to your lower region. What feels different?
- Stay active
- Losing excess body fat can lessen strain on pelvic muscles
- Learn to relax the muscles
- Maintain a fiber-rich diet to prevent constipation
- Seek professional help
Make use of the features on Halza app that can aid better pelvic floor health:
- Health reminders to avoid prolonged seating when working
- Track body fat percentage, weight and other vital signs against lifestyle
- Store, track and share medical records from visits to specialists
- Medication reminders to ensure timely intake of probiotics if suffering from constipation
“Is it too late? Is the damage already done?”
PFD symptoms can be managed regardless of age, gender, and physical trauma. Success of management depends on adequate knowledge and doing the exercises with the correct technique. Some may find the need to speed up the process by increasing the frequency of exercises or treatments. This adds unwanted fatigue to muscles and can increase symptoms.
Seek professional help

As PFD is multifactorial, and requires attention, a pelvic health specialist is best suited to assess and manage your condition.
A health physiotherapist would be able to come up with a tailored program to help prevent the condition from worsening. Many individuals benefit solely from physical therapy.
For those with more severe symptoms and who do not respond well to pelvic floor physical therapy, continence training, or lifestyle modifications, it is best to approach a specialist in gynecology, rehabilitation, or urology. They may carry out further assessments and suggest other possible treatment options such as medications, manipulative interventions and surgery.
How Halza can help?
Manage you and your family’s health easily with the Halza app!
Store, track & share all of your child’s medical records to have them with you, wherever you go. Monitor your child’s growth and vaccination schedule as well as upload reports and doctor’s notes all with the Halza app. QuickShare a complete overview of you or your child’s health with any attending doctor in seconds, during emergencies or whenever you need.
Simplify your health journey with Halza.
Sources: PelvicFloorFirst.org — Continence.org — UrologyHealth.org — UCLA Health