Polycystic Ovary Syndrome: Untangling the Web
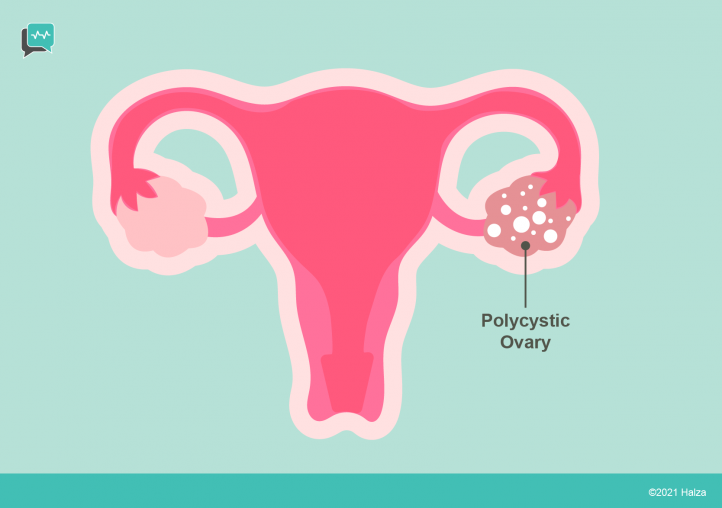
Polycystic Ovary Syndrome (PCOS) affects between six and ten percent of all women and is the most common hormonal disorder among women of reproductive age.
PCOS is usually, but not always, first diagnosed during adolescence, at least two years after the first menstrual period. PCOS affects reproductive, metabolic, hormonal, and cardiovascular functions, among others, and can be life altering. Long term complications can include infertility, diabetes, cancer, and cardiovascular disease.
Scientists do not know exactly why PCOS develops in any one individual. Many different genes, or combinations of genes, have the potential to cause PCOS, and in most cases, environmental factors also play a role. Diagnosis is not always straightforward, in part because symptoms can vary from woman to woman. Up to 80% of women with PCOS are overweight or obese, and lacking that characteristic, diagnosis in lean women may be further delayed until they have difficulty conceiving.
What causes the symptoms and complications of PCOS?

Dysfunctional ovulation
Some symptoms involve dysfunctional ovulation. These include:
- Having irregular periods
- Not ovulating
- Heavy menstrual bleeding infertility having fewer than nine periods per year
- Infertility
- Having fewer than nine periods per year
Endometrial cancer (cancer of the lining of the uterus) can be a long–term complication of having fewer-than-normal periods.
Excessive production of androgens (“hyperandrogenism”)
Some symptoms result from ovarian production of an excessive amount of androgen hormones. Androgens are what we often think of as “male” hormones, like testosterone. In fact, women also produce androgens, but in small amounts.
Symptoms of hyperandrogenism include:
- Hirsutism, which describes the type of hair pattern more typically seen on males. Chest, back and facial hair becomes thick or abundant, while scalp hair becomes thinner and sparser
- Acne
Hyperinsulinemia
Some symptoms result from overproduction of a pancreatic hormone called insulin. Insulin helps glucose enter our cells to provide energy.
For many women with PCOS the cells resist the efforts of insulin. The pancreas is forced to produce extra insulin in order to get glucose into the cells. The overproduction of insulin is called hyperinsulinemia.
In many women with PCOS the extra insulin is still insufficient to get the right amount of glucose into the cells. This is called impaired glucose tolerance, also called prediabetes. Prediabetes can be reversed – or it can become Type 2 diabetes. Type 2 diabetes can lead to cardiovascular diseases such as high blood pressure and heart attacks.
For more information on diabetes see Halza’s article on diabetes here.
How do these conditions relate to weight?

PCOS and risk of weight gain:
PCOS increases a woman’s risk of becoming overweight. Scientists don’t entirely understand how.
Weight and risk of hyperinsulinemia:
Being overweight, with or without PCOS, is a significant risk factor for developing insulin resistance and hyperinsulinemia.
However, even women with PCOS who are not overweight or obese are more likely to develop insulin resistance and hyperinsulinemia than women of similar weight who do not have PCOS.
PCOS and hyperinsulinemia:
In addition to having a higher risk of being overweight, most women with PCOS have more insulin resistance and hyperinsulinemia than what would be expected based on weight alone.
Insulin and androgens:
Insulin stimulates the ovaries to produce androgens.
In women with PCOS, the ovaries are extra-sensitive to insulin. Therefore, the ovaries of a woman with PCOS and hyperinsulinemia (or, of course, PCOS and pre-diabetes or diabetes) will overproduce androgens.
Androgens and the menstrual cycle:
Androgens, together with several other hormones, affect the timing of ovulation and the menstrual period. A regular menstrual cycle relies on these hormones being produced and released at specific times and in specific quantities.
Hyperandrogenism therefore can cause irregular or too few menstrual periods, can prevent ovulation, and, because the uterine lining is shed less often, can increase the risk of endometrial cancer (cancer of the lining of the uterus).
Weight and sleep apnea – one of many other related conditions:
Obstructive Sleep Apnea (OSA) is a condition in which the airway becomes briefly blocked by throat tissue during inhalation. This can happen from a few times to hundreds of times each night. Naturally, people with OSA report feeling tired throughout the day.
Being overweight, as are many people with PCOS, is a risk factor for OSA. Poor sleep is a risk factor for weight gain. Weight gain is a risk factor for hyperinsulinemia. Hyperinsulinemia is a risk factor for pre-diabetes and Type 2 diabetes.
Can losing weight reduce symptoms of PCOS and reduce the risk of diabetes?

Losing even 5-10% of body weight is associated with:
- A more regular menstrual cycle
- A reduction in hirsutism and acne
- A higher likelihood of ovulation
- A reduction in hyperinsulinemia resulting in:
- A reduced risk of Type 2 diabetes
- A reduced risk of cardiovascular disease and other complications of diabetes.
Weight loss can be achieved with lifestyle changes including improved dietary habits and an increase in physical activity. Alternatives include short-term medication and bariatric surgery.
Is it possible to eliminate all of the symptoms of PCOS?

While weight loss can definitely help to reduce the symptoms and complications of PCOS, for some overweight women weight loss alone might not be sufficient, and for lean women weight loss would not be recommended. In these cases, other treatments can be prescribed. Examples include letrozole, a drug used to induce ovulation in women who are pursuing a pregnancy; combined estrogen-progestin oral contraceptives to reduce hyperandrogenism and menstrual irregularities; metformin to reduce insulin levels; dental appliances or CPAP machines to reduce sleep apnea; and psychotherapy or medication to help with symptoms of depression associated with PCOS.
As with any condition, everyone responds differently to treatment, and it can take some time and effort to find the best combination of drugs, lifestyle changes and other therapies. But with that effort, and with access to treatment, most women will find that their symptoms of PCOS can be significantly reduced.
How Halza can help?
Manage your family’s health easily with the Halza app. Store, track & share all of your child’s medical records to have them with you, wherever you go. Monitor your child’s growth and vaccination schedule as well as upload reports and doctor’s notes all with the Halza app. QuickShare a complete overview of you or your child’s health with any attending doctor in seconds, during emergencies or whenever you need.
Simplify your health journey with Halza.