All You Need to Know About Non-Alcoholic Fatty Liver Disease

Has your doctor told you that you or a loved one has Fatty Liver Disease and that you should lose some weight?
Did you go home and google what the functions of the liver are?
If you did, you probably learned that the liver is responsible for many different functions, including:
- filtering toxins from the blood
- making proteins
- processing nutrients from food
- making bile, a substance that helps us digest fat
- storing glycogen, a major source of energy
- metabolizing medication
But then…did you google Fatty Liver Disease?
Did your head spin as you read about Hepatic Steatosis, Steatohepatitis, NASH, Cirrhosis, Fibrosis, Metabolic Syndrome, Hypertriglyceridemia, and lots of other unfamiliar words?
Don’t worry. By the time you finish reading this article, it will all be clear.
First, let’s take the mystery out of the term Hepatic Steatosis.
“Hepatic” refers to the liver.
“Steat” refers to fat.
“…osis” is a suffix that refers to a certain condition or state.
If you put them together, you get “Hepatic Steatosis”, which just means “Fatty Liver!
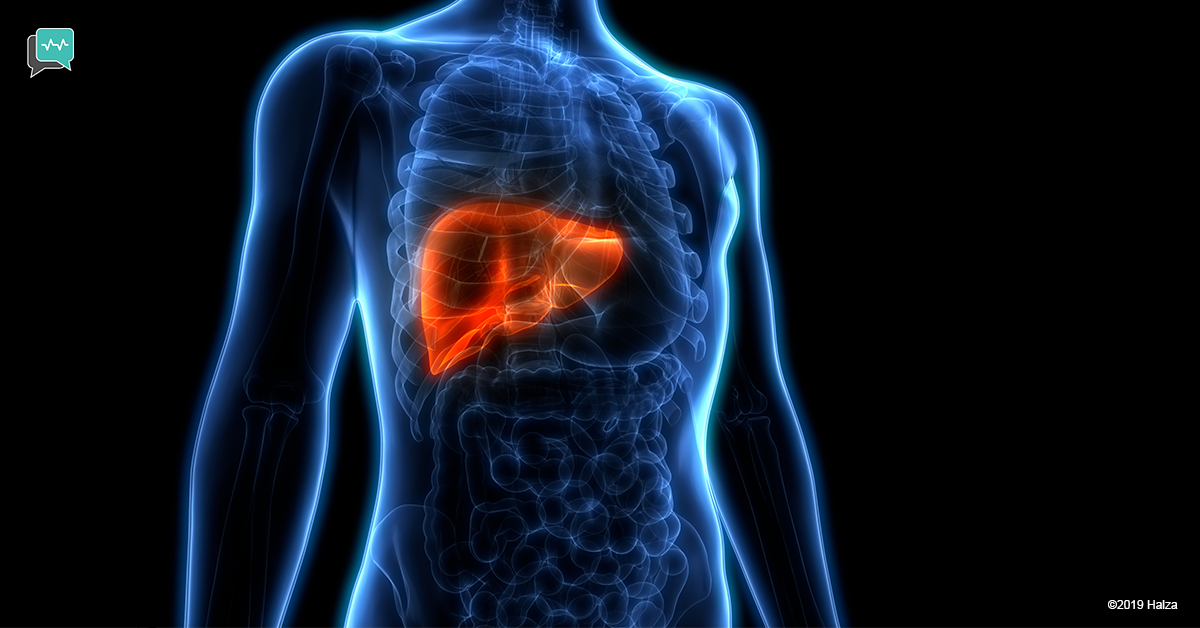
Every healthy liver has a small amount of fat in it, necessary for functioning. But having more fat than necessary can – but does not always – lead to complications. Though there is no single medical cure, the good news is that a fatty liver can be managed and often resolved through treatment.
Why is it called non-alcoholic fatty liver disease (NAFLD)?
This is to distinguish it from Alcoholic Fatty Liver Disease (AFLD), which eventually affects all heavy drinkers.
But roughly 30% of all adults in Europe and the United States and 15-20% of adults in Asia, who are not heavy drinkers, or don’t ever drink alcohol, will also develop Fatty Liver Disease.
The progression of AFLD and NAFLD and the recommendations for treatment are different.
I must know people who have this. Why don’t they seem to be sick?
Unlike with other liver diseases, most people with NAFLD don’t feel sick or have any symptoms of liver problems. Although the liver has excess fat, the fat is not causing any problems. This is called Simple Fatty Liver. The liver is able to deal with the extra fat by repairing or regenerating healthy cells.
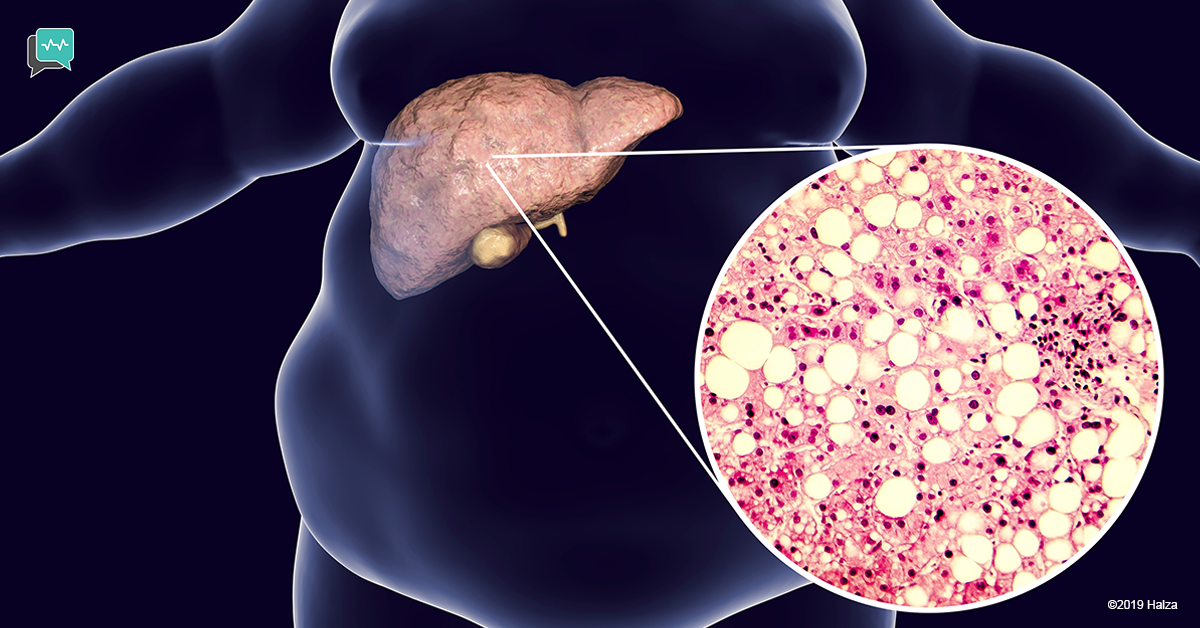
However, in some cases the excess fat, mostly in the form of triglycerides, causes inflammation. This condition is called NASH, for “Non-alcoholic Steatohepatitis”.
(Note: “…itis” is a suffix that refers to inflammation. So “hepatitis” is an inflammation of the liver. If you put hepatitis together with “steat”, you get steatohepatitis: a fatty liver with inflammation.)
The liver responds to inflammation by attempting to repair or regenerate liver cells. This process causes scar tissue to form, called “fibrosis”. The scar tissue takes the place of healthy liver cells.
If NASH is not treated, scar tissue (fibrosis) continues to build up as the liver tries to regenerate its cells.

When the liver can no longer regenerate healthy cells because of all the scar tissue, the condition is called “cirrhosis”. If the underlying causes of cirrhosis are not treated and damage to the liver continues, liver failure will occur.
We don’t know exactly why some people with NAFLD develop the inflammation of NASH while others don’t.
Who gets fatty liver disease?
People who get Alcoholic Fatty Liver Disease are by definition, heavy drinkers.
Virtually anyone can get Non-Alcoholic Fatty Liver Disease, including children.
It is the most common liver disorder in the world, and it is found in all races and ethnicities. It can be diagnosed at any age. Men and women are affected roughly equally.
However, the vast majority of people with NAFLD have one or more of a few specific risk factors related to Metabolic Syndrome.
Metabolic Syndrome refers to having three or more of the following conditions. The risk factors are:
- obesity, particularly a large waist circumference
- high blood sugar
- abnormal cholesterol levels
- high blood pressure
- hypertriglyceridemia
(Note: “hyper” means too high. “triglyceride” refers to a type of fat from extra calories “emia” means in the blood. So, hypertriglyceridemia means that the level of triglycerides in your blood is too high.)

People with Metabolic Syndrome are at high risk of developing cardiovascular disease and/or diabetes.
All the conditions of Metabolic Syndrome are closely linked with excess weight and occur more frequently as countries become more industrialized.
How are NAFLD and NASH diagnosed?

NAFLD and NASH can be diagnosed through a combination of the following.
Through your Medical History
The doctor will look for risk factors or symptoms such as:
- pre-existing medical conditions you might have
- high intake of alcohol (to rule out a diagnosis of Alcoholic Fatty Liver Disease)
- an unhealthy diet or eating habits
- a low level of physical activity
- a family history of liver disease or conditions related to NAFLD
- certain medications
- feeling fatigued
With a Physical Exam
This helps determine if you have any signs of liver disease or of risk factors related to Fatty Liver Disease, such as:
- being overweight, especially in the abdomen
- high blood pressure
- an enlarged liver
- fluid in the abdomen
- dark patches of skin suggesting insulin resistance
- jaundice
Medical Tests
These include:
1. Blood tests
- cholesterol levels
- triglyceride levels
- blood sugar
- liver function tests.
- tests to rule out other medical conditions
2. Non-invasive imaging
- Ultrasound
It can show the size and shape of the liver and how well blood is flowing through. It can also show if a liver is fatty or if cirrhosis (advanced fibrosis) is present.
- CT scan
Like ultrasound, the CT scan show if a liver is fatty or fibrotic. A CT scan will produce clearer images than ultrasound; however, the patient is exposed to radiation.
- MRI
It will pick up even low levels of fat in the liver. Some imaging centers use a technique that shows what percent of the liver is fat.
- Elastography
Done during an ultrasound or MRI. Elastography measures the stiffness (or elasticity) of the liver. Fibrotic livers are stiffer than healthy livers. Elastography can usually detect fibrosis earlier than other imaging techniques.
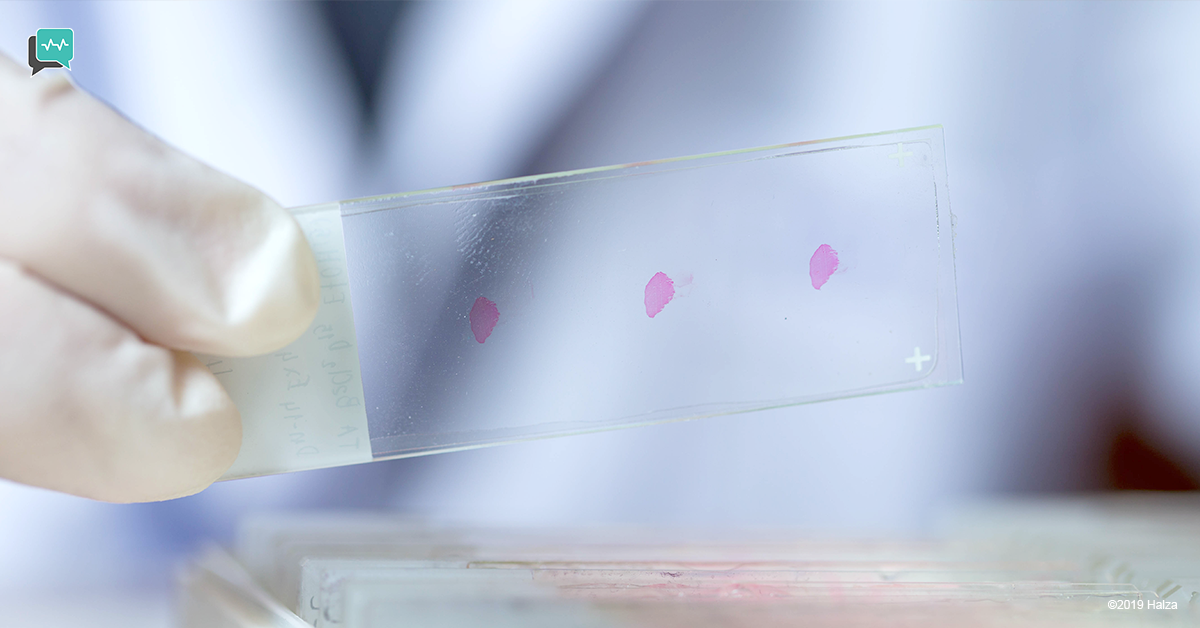
3. Liver biopsy
In a liver biopsy, the patient is given a local anesthetic (and sometimes a sedative) and the doctor inserts a needle into the liver to remove a tissue sample. The sample is sent to a pathologist and examined under a microscope.
This is currently the only way to definitively determine if inflammation is present and if so, the likely cause.
How are NAFLD and NASH treated?
Simple Fatty Liver and NASH are treated by minimizing the underlying risk factors.
Most of the factors related to Metabolic Syndrome are improved by losing weight. Simple Fatty Liver may react to a weight loss of 3-5% of body weight, while up to 10% weight loss might be recommended to minimize the inflammation of NASH.
A reasonable guideline is to lose not more than 2-4 kilograms per week by:
1. Increasing activity levels as per your doctor’s recommendation, and
2. Following a healthy diet with reduced portion sizes. Be aware that rapid weight loss can actually contribute to NAFLD.
A healthy way of eating for almost everyone, but particularly for someone with risk factors for Metabolic Syndrome, is the Mediterranean Diet.
Follow your doctor’s advice regarding alcohol, which may be good for the heart but stressful for the liver. Medication may be prescribed to reduce cholesterol or blood sugar levels if they are too high.

There is currently no medication specifically designed to treat NAFLD, although a few medications to treat other conditions may additionally benefit the liver in specific populations.
Studies for new medications are ongoing, so ask your doctor if you might be eligible for a clinical trial.
If cirrhosis is not treated and enough of the liver becomes damaged to the point of not functioning, called liver failure, a liver transplant is needed.
If your Fatty Liver Disease is caused by a reason not related to factors of Metabolic Syndrome, your doctor will advise you on the appropriate treatment.
How can I prevent NAFLD?

To minimize your risk of developing NAFLD, follow a lifestyle that minimizes the risk of obesity and other factors related to Metabolic Syndrome.
- Eat a healthy diet, such as the Mediterranean Diet, which emphasizes on low-fat sources of protein such as poultry and fish, carbohydrates from beans, and fresh fruits and vegetables, and fats from poly or mono-unsaturated oils. It also includes Omega-3-rich fish like salmon and mackerel.
- Unless your doctor has advised against it, regularly exercise for 30 minutes, five times per week.
- Ask your doctor if you have any risk factors, including any medications you are taking.
Doctor: I’m sorry to tell you that you have hepatic steatosis with steatohepatitis and mild fibrosis because of metabolic syndrome and hypertriglyceridemia.”
You: “You mean that I have a fatty liver with some inflammation and scarring but I can treat it by reducing my risk factors for diabetes and heart disease?”
Doctor: Yes, that’s what I meant to say. Thank you.
How Halza can help
Manage NAFLD with the Halza app! Store, track & share your medical records, including ultrasounds, CT scans, MRIs, and liver biopsies, all from the palm of your hand.
Track your liver function and get a quick overview of Vital Signs on your dashboard. Set weight goals and meet them by leaving yourself messages of encouragement with the Weight Management feature.
Set medicine and health reminders to ensure you never miss a medicine dose or a scheduled appointment.
The Halza app is also available in 26 languages.
Download now!
Sources: Healthline – Mayoclinic – Nature Reviews – NCBI – Harvard Health [/vc_column_text][/vc_column][/vc_row]